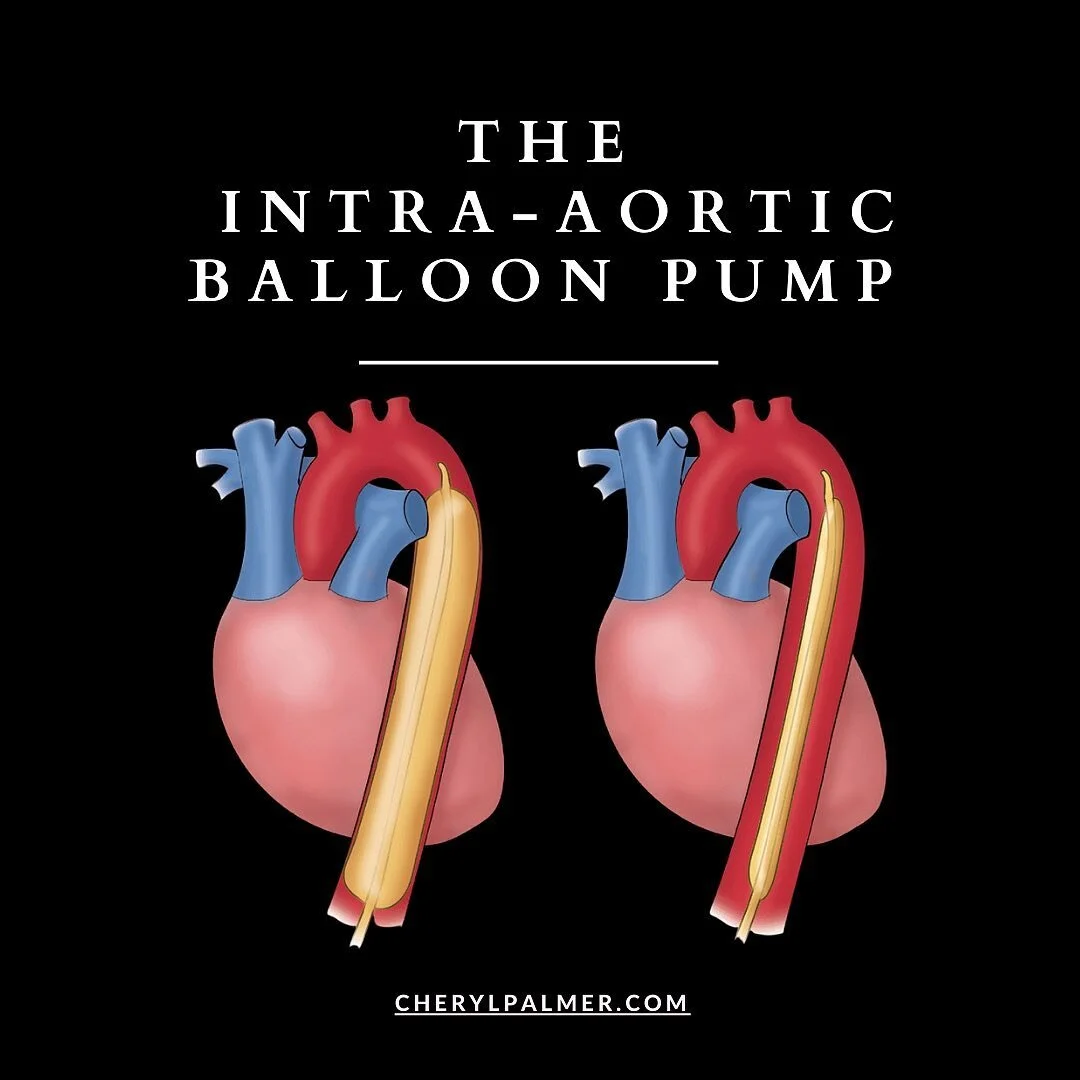
The Intra Aortic Balloon Pump
The intra-aortic balloon pump (IABP) is a volume displacement device positioned between a left subclavian artery and renal arteries. The usual insertion site is the femoral artery but the balloon may also be inserted via the aortic arch, common iliac, subclavian, axillary, or brachial arteries. With the EKG or arterial pressure wave as a signal, the IABP is timed to synchronize with the cardiac cycle to inflate during diastole and deflate during systole. In summary, the balloon inflates in diastole, displacing aortic blood both into the systemic circulation and into the coronary arteries. The balloon deflates before systole, decreasing aortic pressure. Diastolic augmentation thus improves coronary blood flow. Systolic augmentation thus decreases afterload and LV workload.
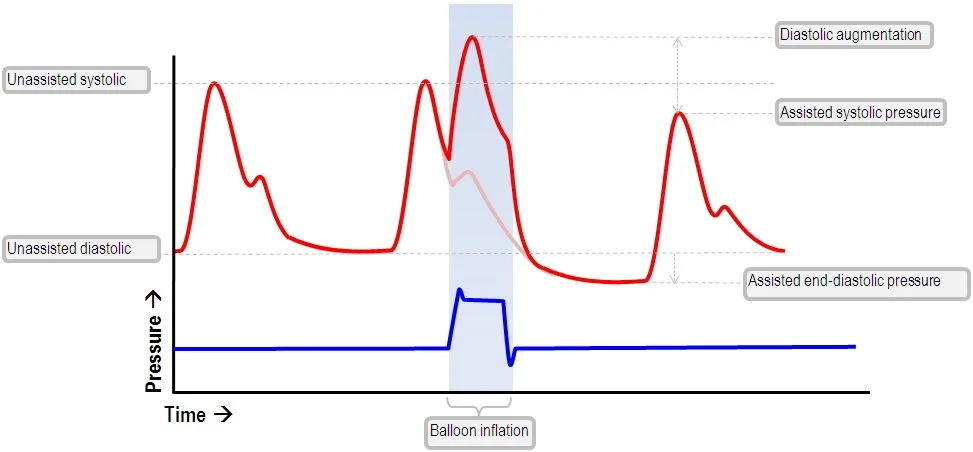
Inflation during Diastole
Inflation is said to occur at the start of diastole, the point in time when 75 to 90% of coronary artery perfusion occurs. The increase in early diastolic pressure in the aortic arch increases coronary artery perfusion and increases myocardial oxygen supply. Balloon inflation also increases perfusion pressure below the balloon, thus increasing forward flow, peripheral perfusion, and peripheral blood pressure.
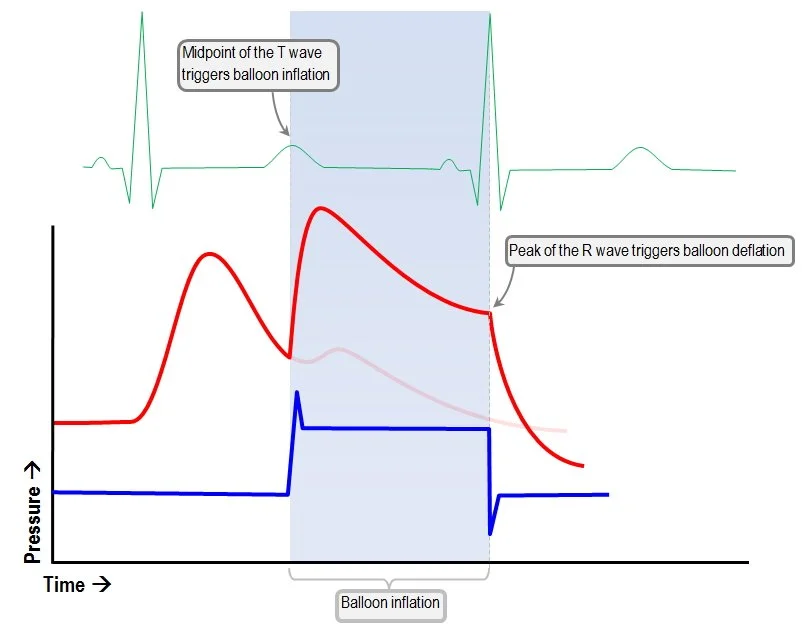
The increase in early diastolic pressure by the balloon is referred to as diastolic augmentation. Diastole begins with the closure of the aortic valve, which creates to dicrotic notch on the arterial wave. The dicrotic notch is the best marker for timing balloon inflation. Balloon inflation must occur prior to the next systole. Deflated during systole. Deflation is said to occur at the end of diastole during the period of isovolumetric contraction when all the cardiac valves are closed.
Just as the aortic valve opens, the deflation-induced reduction in aortic root pressure presents the left ventricle with less pressure against which to eject. This translates into less ventricular wall stress, lower afterload, and decreased heart work and myocardial O2 demand (MVO2). The positive effects of decreased stress during systole are revealed by a decrease in peak systolic pressure.
Systole begins when the systolic upslope begins Deflation should occur slightly before the beginning of the systolic upslope. The balloon must remain deflated throughout the systolic period.
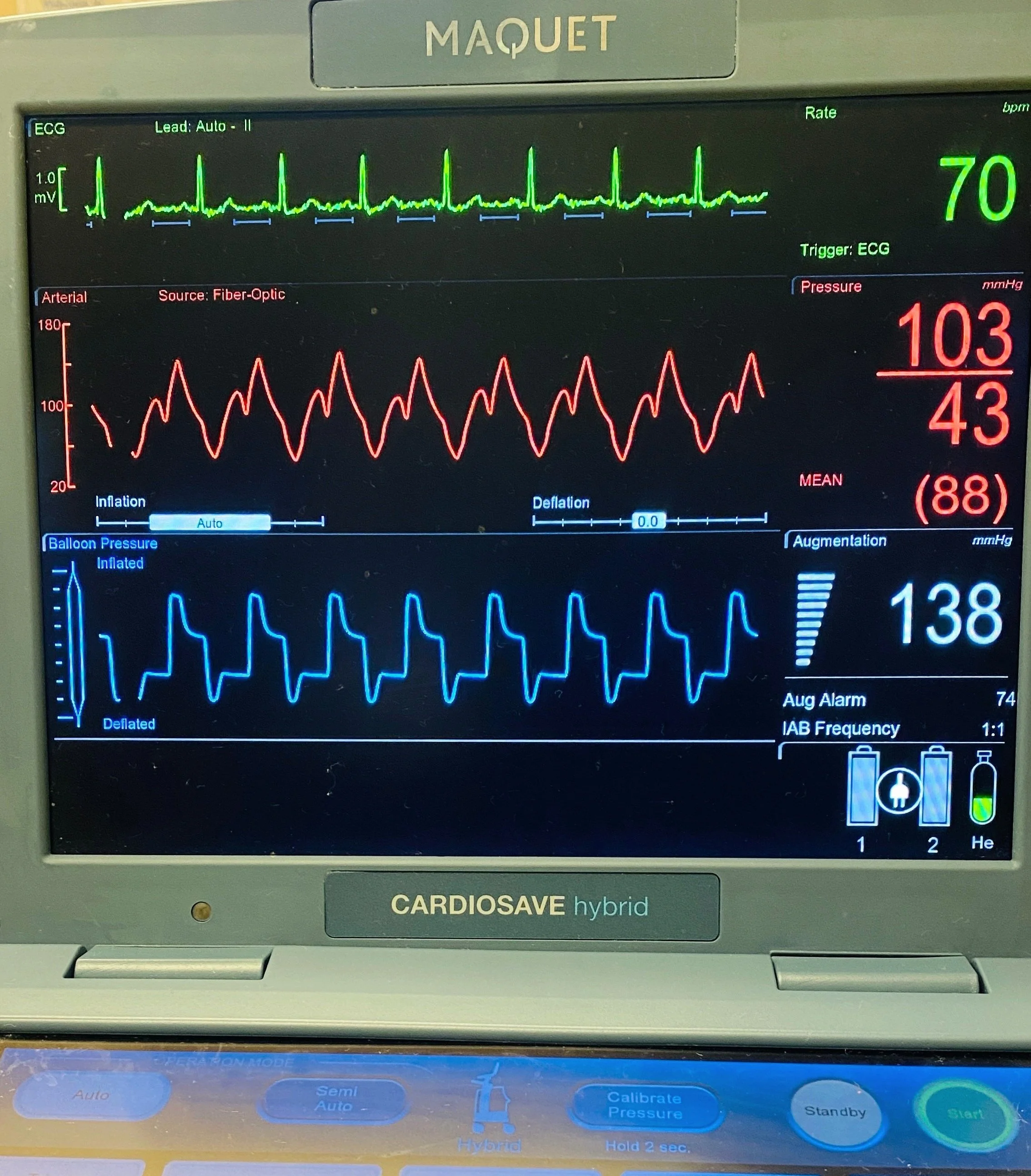
Normal IABP Waveform
ECG triggering of the IABP
Therapeutic goals of IABP
Improved mean arterial pressure cardiac output heart rate and rhythm
Decreased Pulmonary capillary wedge pressure
Decreased systemic vascular resistance
Improved renal function
Improved oxygenation
Resolved myocardial ischemia
What do I need to KNOW?
The frequency of IABP must be ordered as 1:1, 1:2, or 1:3
When should the IABP be placed on Standby?
When clinicians are listening to heart sounds
During Chest X-Ray
When credentialed prescriber is adjusting the placement of the IABP
When RN is flushing the IABP catheter Q 1 hours
NEVER leave the IABP catheter on Standby for > 30 minutes or it must be removed
What do I need to DO?
Check patient’s pulses every hour with IABP pumping both distal to the IABP catheter as well as left brachial or left radial pulse.
NS flush bag should be at 300 mmHg
NS flush bag should be 3 feet above the IABP catheter insertion site
If ordered, Heparin flush is 2000 units of Heparin/1000 ml of NS
Check hemodynamic numbers immediately after a change in the IABP frequency
Benefits
The balloon inflates in diastole, displacing aortic blood both into the systemic circulation and into the coronary arteries.
The balloon deflates before systole, decreasing aortic pressure.
Diastolic augmentation thus improves coronary blood flow.
Systolic augmentation thus decreases afterload and LV workload.
Absolute Contraindications
Aortic regurgitation
Aortic aneurysm
Aortic dissection
Severe sepsis
Uncontrolled coagulopathy
Relative contraindications
Atherosclerosis and arterial tortuosity
Left ventricular outflow tract obstruction
Contraindications to anticoagulation
Common complications
Mild limb ischemia - 2.9%
Balloon leak - 1.0%
Major limb ischemia - 0.9%
Hemorrhage - 0.8%
Leg amputation due to ischemia - 0.1%
Rare complications
Atheromatous cholesterol emboli
Aortic or arterial dissection
Cerebrovascular accident
Thrombocytopenia
Hemolysis
Helium embolism
References and Resources:
IABP Waveforms